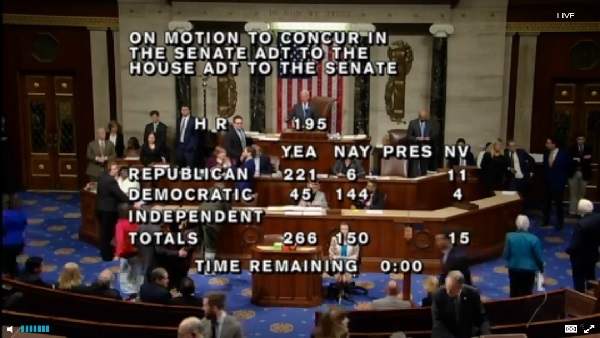
 President Donald Trump has signed an anti-government shutdown bill that will eliminate $12.7 billion in Affordable Care Act health insurer fee taxes for 2019.
President Donald Trump has signed an anti-government shutdown bill that will eliminate $12.7 billion in Affordable Care Act health insurer fee taxes for 2019.
The new “Extension of Continuing Appropriations Act, 2018″ (ECAA) will also:
- Give the federal government official permission to spend money, and continue with normal operations, until Feb. 8.
- Extend funding for the Children's Health Insurance Program for six years.
- Push the scheduled start date of the ACA Cadillac plan tax, or 40% excise tax on high-cost employee health benefits packages, back to 2022, from 2020.
- Suspend collection of the ACA medical device tax for two years.
Congressional Budget Office analysts have predicted the health insurer tax and Cadillac plan provisions will reduce federal revenue by a total of about $29 billion over 10 years.
A summary of the bill posted last week is available here.
Complete your profile to continue reading and get FREE access to Treasury & Risk, part of your ALM digital membership.
Your access to unlimited Treasury & Risk content isn’t changing.
Once you are an ALM digital member, you’ll receive:
- Thought leadership on regulatory changes, economic trends, corporate success stories, and tactical solutions for treasurers, CFOs, risk managers, controllers, and other finance professionals
- Informative weekly newsletter featuring news, analysis, real-world case studies, and other critical content
- Educational webcasts, white papers, and ebooks from industry thought leaders
- Critical coverage of the employee benefits and financial advisory markets on our other ALM sites, PropertyCasualty360 and ThinkAdvisor
Already have an account? Sign In Now
*May exclude premium content© 2025 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.